The End IS Near. No, Seriously.
The tone of some recent writing about this pandemic has seemed — to me, anyway — strangely defeatist.
Friends keep asking me questions like: “Is what I’m hearing true? We’ll never reach herd immunity?”
The subtext is we’ll never really be safe, we dare not demask, the pandemic will never leave us. It’s almost as if some writers are reluctant to let go of the biggest disaster (and biggest story) of our lives.
We should be clear about this: our Great National Misery is ending.
All epidemics end, vaccine or no vaccine. The Spanish Flu ended. The Black Death ended.
And yes, in those cases, herd immunity did it. We reached it the hard way — down the stone paths in the cemeteries— but we got there.
But herd immunity is not the whole picture. Nor is it what constitutes “the end.”
By that I mean: the Black Death and the Spanish Flu ended only as epidemics.
The pathogens that caused them didn’t vanish. They’re still with us. But you don’t need transmission exterminated to say an epidemic is over. You just need it manageable.
Herd immunity is not a moment in time. President Biden is never going to say: “Today, at 9:04 A.M., on the deck of the U.S.S. Moderna, the virus known as SARS-CoV-2 signed our general terms of surrender.”
Instead, this virus is slowly becoming endemic: something we live with.
We will probably have bad seasons and good seasons, as we do with flu. We may have annual shots with a blend of the South African, Brazilian, Indian or whatever variants are circling the globe that year. Luckily, because coronaviruses mutate more slowly than influenza viruses, they will probably be better matches than flu shots are.
But the epidemic-endemic border is fuzzy. My epidemic may end before yours does.
Our national herd has many sub-herds. Immunity’s growth rate is variable, not just state by state, but block by block, and profession by profession. Front-line nurses and meatpackers, homebound software engineers and transitioning schoolteachers are all increasing their immunity levels by different routes.
We are already a good way down the yellow brick road back to Normal.
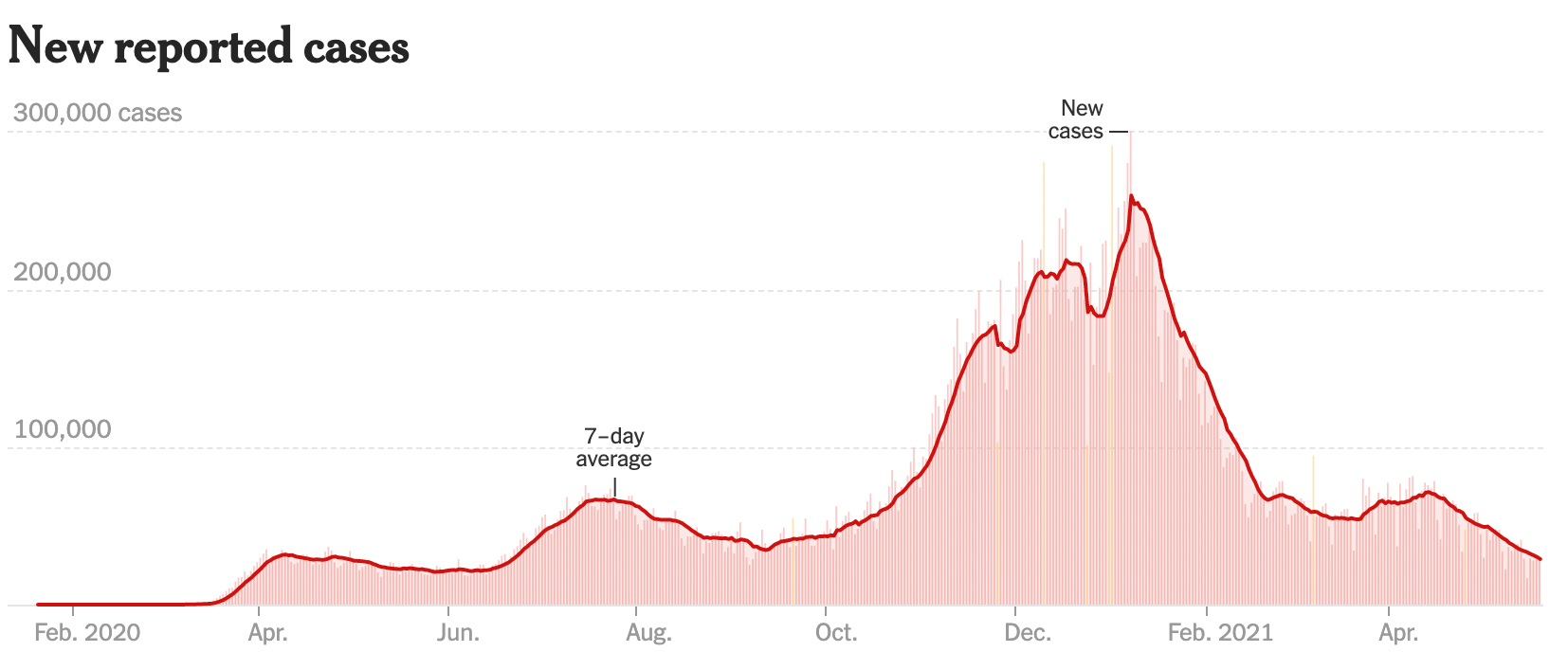
Cases are going down steeply again. The late March surge caused by the rapid spread of the British variant was beaten back. It looks like we sped up vaccinations enough to outrun it; about 61 percent of us have had at least one dose.
The other variants are here, but they’re not spreading as quickly. We the vaccinated plus we the survivors are acting like the boron rods in a nuclear reactor: impervious or mostly impervious to the virus, we are absorbing the virions but not retransmitting them, thereby preventing chain reactions. (Have you noticed that reports of superspreader events have really fallen off?)
Hospitalizations — a more reliable measure than positive tests — are also going down again.

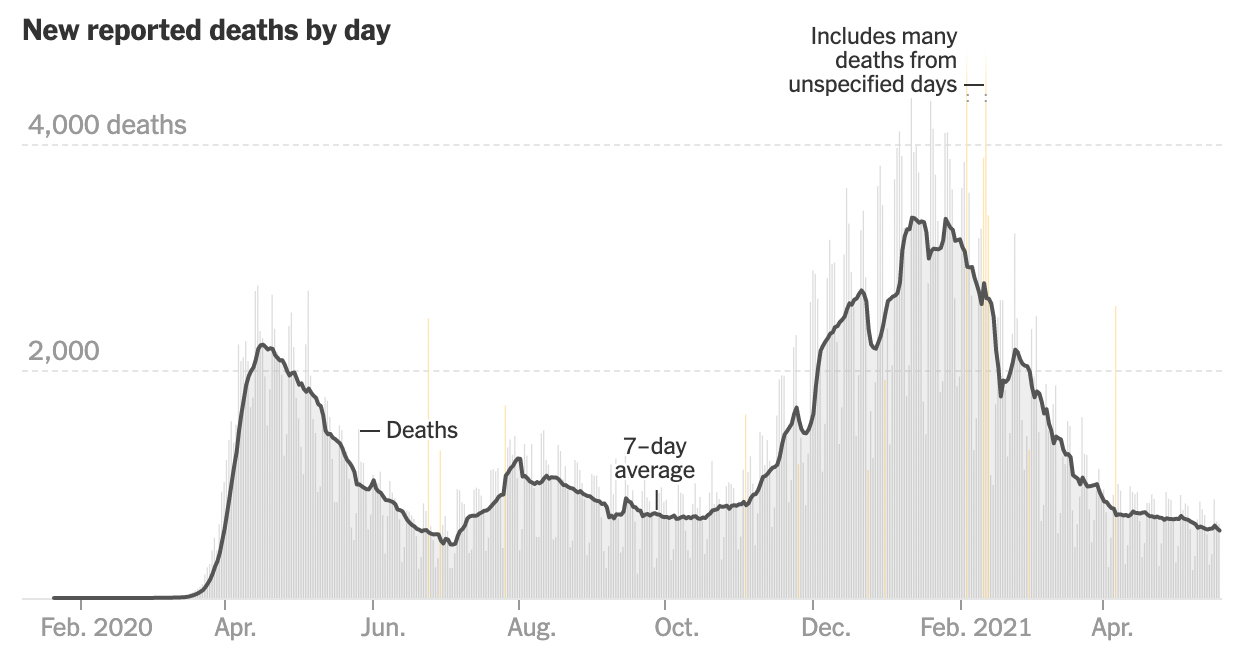
Deaths are still pretty flat. But they always lag cases and hospitalizations by weeks.
Normality is on the way.
So what’s “normal”? Shopping without masks? Hugging your grandchildren? Taking a flight? Catching a movie? Breaking up your pod? Reading a newspaper that doesn’t contain a single Covid-19 story?
Yes, all of the above. But they all boil down to the same thing: “normality” is actually not a number like 85 percent immune. Normal means we’ve reached a risk-of-illness-or-death level we can accept.
Epidemiology isn’t the only science that dictates when pandemics end. Psychology plays a big role.
With flu, “normal” is 12,000 to 60,000 dead per year. Some of us know that, some of us don’t. As a result, some of us get flu shots, some of us don’t. Maybe in the future, some of us will wear masks in December and January and some of us won’t.
But at some point, we each individually decide “OK, I can live with this much risk.” Then peer pressure kicks in. “Well, if you can, I can too.”
It’s already started. I live in an aggressively mask-affirmative Brooklyn neighborhood. But just in the last couple of weeks, I’d say that roughly 20 percent of the masks have come off — on the sidewalks, that is.
Demasking indoors is still in transition: in restaurants yes, in grocery stores no. That makes little sense, but it’s how it is. Now even Trader Joe’s says it will ease up on masks, though some of my neighbors are clearly unhappy about that.
At what point do we accept our illness-or-death risk? That’s not a collective decision. It’s an individual one.
I’m already eating at the bar at my corner beer-and-burger joint again.
On the other hand, I’m not willing to fly to India just now. Not as much out of fear of Covid but because, if I happened to have, say, a heart attack, I clearly would be unable to get a hospital bed or an oxygen mask.
Perception of risk is everything. Consider this: about 3 million Americans die each year. (TW//: We all have to die of something.)
In most years, we shuffle off this mortal coil due to, in this order: heart disease, cancer, accidents, COPD, stroke, Alzheimer’s, diabetes, kidney failure, flu/pneumonia and suicide.
Last year, despite all the ink spilled on it, Covid-19 was our leading cause of death only in some weeks. I vividly remember when it first hit № 1: it was on April 7. Nonetheless, it still ended 2020 at just № 3, after heart disease and cancer.
This year, because the January-February surge was so bad, it will probably be № 3 once more. But never again after that. Too much immunity, not enough kindling left for another firestorm.
However, please note: with the exception of Alzheimers and freak accidents like lightning strikes, almost all those top 10 causes of death are abetted by risks some of us long ago rationally (or semi-rationally) decided to accept: smoking, drinking, overeating, driving, kissing, chainsaw-juggling and so on.
Risks increase with age: no one dies at age 13 from their first cigarette. Covid death risk also increases with age; our national nervousness is age-stratified. (We know this from watching the average age of hospital admittees drop.)
Flu, at № 9, is the closest thing on the American mortality list to Covid-19. We all know how to minimize our flu risk — flu shots. But many of us don’t bother. We accept what we perceive to be our risk. Flu is objectively scary — but we aren’t very scared.
Thus will it soon be with Covid-19.
My own herd — my friends, my family, my softball team — has very high levels of immunity. Almost everyone I know over age 12 has had the shots.
I’m guessing the same about my neighbors. But I know that in some Brooklyn neighborhoods within a mile or two of me, vaccination rates are far lower. In rural America, they are even lower — partly because of lack of access but now often from choice.
Those are the weak spots the virus is still slithering into, raising herd immunity the old fashioned way: the diehards die hard, the survivors become insulators.
(Another group remains vulnerable, though not by choice: the 10 million Americans who are on immunosuppressive drugs because they have had organ transplants, are fighting cancer or have autoimmune diseases like rheumatoid arthritis or lupus. But it’s possible that extra booster doses will protect them — which would make sense since stronger shots protect older people against flu and hepatitis B.)
History also suggests the end is near.
Our closest model to this pandemic, the 1918 flu, had a huge fall-winter surge of deaths, just as we did. Then it had a third surge in its second spring — a fate we appear to have dodged.

Remember, even the Black Death never completely ended; Yersinia pestis, the bacterium that caused it, is still circulating. Every year, it claims some unlucky victims. Most often in Madagascar, sometimes in Mongolia — and even inside the United States. Y. pestis is endemic in marmots in Mongolia, rice rats in Madagascar and prairie dogs and squirrels here.
Herd immunity — rather than a change in rat or flea populations, for example — probably triumphed even over plague. In 1382, Raimondo Chalmel de Vinario, the Pope’s house physician in Avignon, noted that, when the 1347–48 plague returned in waves in 1362, 1371 and 1382, it killed a smaller proportion of its victims each time. By 1382, it was mostly a disease of children; adults were presumably immune.
(In subsequent centuries, plague returned intermittently, killing people of all ages. But it tended to pop up in one spot or another, like London or Milan, rather than going pandemic.)
Now, without either a vaccine or herd immunity, we do not fear a plague epidemic. Why not? Because we have a cure: antibiotics. We know we can stop an outbreak in its tracks.
That also needs to be taken into account in this pandemic: cures don’t affect herd immunity levels at all. But they do cut death rates. And when you fear death less, you behave more normally.
We don’t have a fool-proof cure for Covid, but we have an excellent treatment: monoclonal antibodies. A recent study showed them cutting hospitalization and death by 71 percent even in in high-risk patients. An earlier study showed an 80 percent reduction in severe disease in nursing home patients.
Also, so many doses are now available that they are being pushed on TV. As in: “if you’ve tested positive for Covid, ask your doctor about monoclonal antibodies.” As more patients learn to ask for them immediately, and as prescribing them becomes more routine for doctors, death rates will drop even faster.
And that — the vague but calming sense that our own death is no longer imminent — is what is going to let each of us say, in our own moment of epiphany: “Hey — I suddenly feel like it’s over.”
And when enough of us do — it will be.
https://donaldgmcneiljr1954.medium.com/the-end-is-near-no-seriously-142683fb085e



No comments:
Post a Comment